Dry Eye Syndrome
Erosion of corneal epithelium owing to inadequate hydration
Attributed to autoimmune attack on lacrimal glands, often part of Sjogren syndrome (“keratitis sicca”)
Affects patients of all ages, but mostly middle-aged and older women
Mild cases are successfully treated with tear replacement eyedrops
Severe cases may require more aggressive measures to preserve normal tears, protect cornea from exposure, reduce inflammation of lacrimal glands
Patients report “foreign body sensation” exacerbated by corneal exposure and dry climates
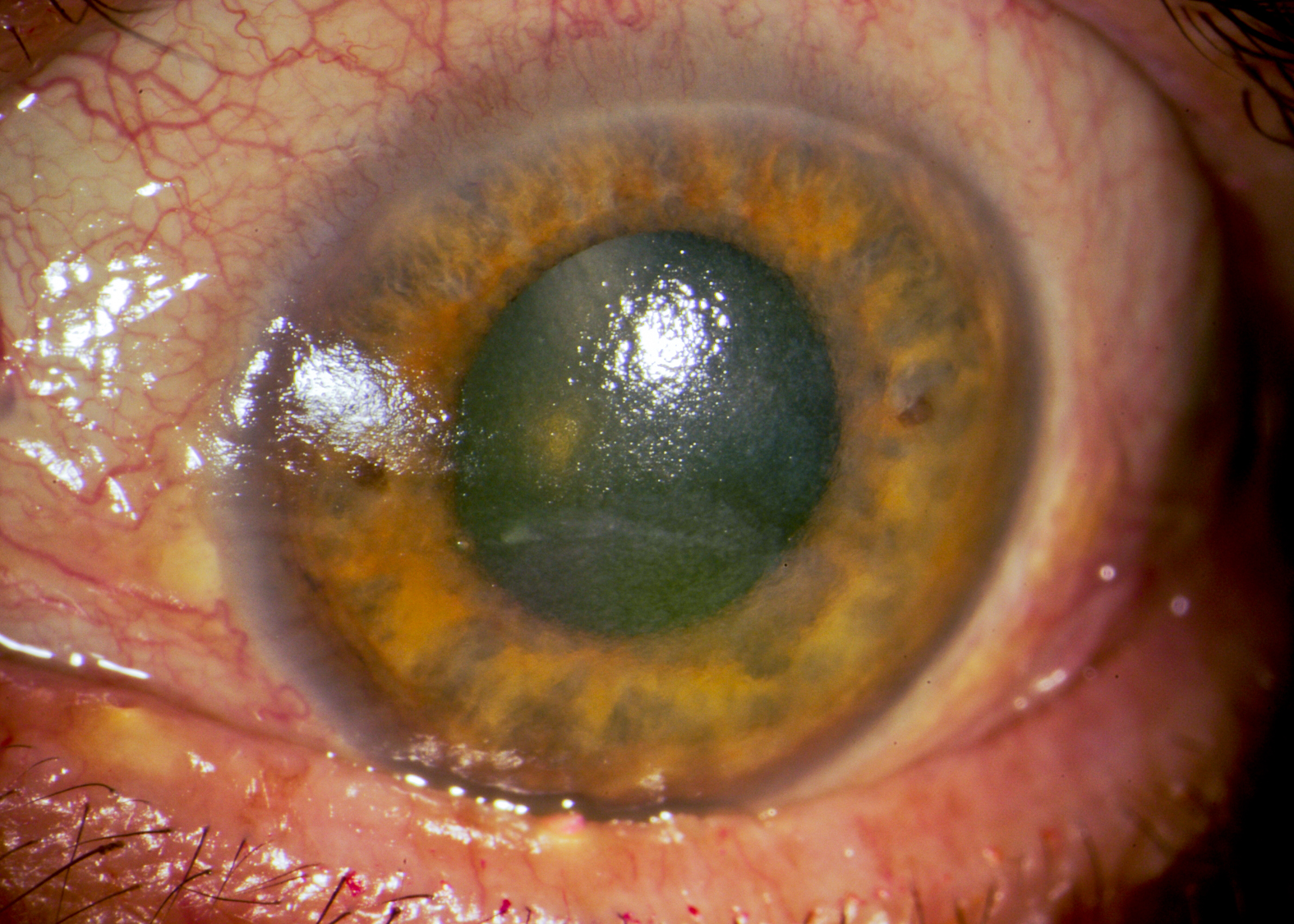
Conjunctival hyperemia, usually mild, and concentrated around limbus (“ciliary flush”)
Normally smooth light reflection on cornea appears “broken up”
Areas of denuded corneal epithelium stain with topical fluorescein
Punctate areas of dehydrated conjunctiva stain with topical Lissamine green
Tear “break-up time” is decreased
Sebum from engorged meibomian glands sometimes appears on lid margins
Visual acuity will be impaired if corneal epithelium in optical axis is eroded
May be associated with systemic autoimmune disorders, especially Sjogren syndrome
Allergic and viral conjunctivitis
Keratopathy of many different causes, including herpetic, exposure, toxic, inflammatory, traumatic, denervation
Establish underlying cause
Treat with tear replacements (“artificial tears,” “tear substitutes”), initially choosing over-the-counter non-viscous formulations, working up to more viscous formulations as needed
Prescribe preservative-free, single-dose formulations if patient does not tolerate standard formulations
If these remedies do not work, refer to an ophthalmologist
Most patients achieve symptom relief with standard tear substitutes
If patient does not achieve symptom relief, refer to an ophthalmologist